What’s the diagnosis?
Alopecia with broken hairs

Figure 1. Alopecia demonstrating irregular margins with partial regrowth and broken hairs of uneven length.
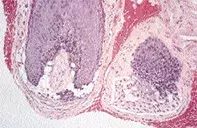
Figure 2. Scalp biopsy showing clefts, haemorrhage and focal necrosis at the level of the follicular bulbs.
Differential Diagnosis
Alopecia areata is characterised by circumscribed areas of hair loss which may become extensive. Partial hair regrowth, lack of erythema and black dots may be seen. The broken hairs in alopecia areata are tapered at the scalp (exclamation mark hairs). Scalp biopsy shows miniaturised hair follicles with peribulbar inflammation without clefting or haemorrhage.
Tinea capitis may present with alopecia, broken lustreless hairs and black dots. Careful examination may reveal scaling or pustules. Wood’s UV light examination may show positive green-yellow fluorescence. Extraction of the broken hairs usually reveals fungal elements that can be cultured.
Trichotillomania (compulsive hair pulling) is the correct diagnosis and represents an impulsive disorder of hair plucking. Clinical examination reveals broken hairs, and scalp biopsy may demonstrate evidence of avulsion injury to hair follicles. Patients usually do not admit to hair plucking. Some patients may swallow hairs and develop trichobezoars. Psychological support and an analysis of events that may have triggered this self-induced disorder are required. In children the disorder is usually self-limited. Habit reversal and clomipramine or fluoxetine have been used in adults, with variable benefit.
A 33-year-old woman gave a 12-month history of an extending alopecia (Figure 1). Scalp examination revealed no erythema, pustules or scarring. There were broken hairs and black dots within the follicular orifices. The balding patch had an irregular margin and there were areas of partial hair regrowth. Scalp biopsy showed a normal number of hair follicles. Several follicular bulbs had clefts associated with haemorrhage and focal necrosis (Figure 2).

