What’s the diagnosis?
Asymptomatic annular lesions

Figure 1. Annular plaques on the patient’s hand.
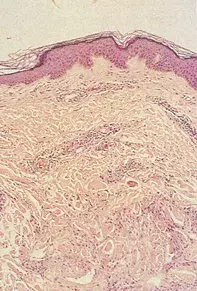
Figure 2. Skin biopsy showing interstitial infiltrate of histiocytes with degeneration of collagen and surrounding perivascular lymphocytic inflammation.
Differential Diagnosis
Tinea may present with annular lesions, but these are associated with scaling as well as pustules. A skin scraping or biopsy will reveal fungi that can also be cultured.
Urticaria is associated with pruritic annular lesions that are rapidly changing. Skin biopsy shows perivascular lymphocytic inflammation with eosinophils.
Annular erythema is a term given to a group of skin conditions associated with expanding erythematous rings that last weeks to months. The rings may be superficial and associated with scaling or they may be deeply set. The annular rims usually expand slowly, leaving central clearing of the skin. Biopsy shows a perivascular lymphocytic infiltrate that may be superficial or deep.
Tuberculoid leprosy is associated with single or multiple annular lesions. Central hypopigmentation and impaired sensation may be clues to diagnosis, as well as palpable near-by peripheral nerves. Biopsy shows perineural granulomas.
Granuloma annulare is the correct diagnosis in this case. This condition presents as asymptomatic annular lesions with erythematous papular rims or as subcutaneous nodules. The pathogenesis remains unknown and appears to represent a dermal form of delayed hypersensitivity reaction associated with collagen damage. Usually there are no systemic associations. Intralesional steroids (such as triamcinolone acetonide) have been used for localised lesions. Potent topical steroids can be applied twice daily. For generalised lesions, dapsone 100 mg daily, oral prednisone 25 mg daily or oxpentifylline 400 mg three times a day have been used for periods of four to 12 weeks with variable success.
Over a 12-month period, a 52-year-old woman developed a series of asymptomatic annular lesions, measuring 2 to 6 cm in diameter, on her limbs (Figure 1). There was no scaling, and the lesions had increased in number and size gradually without resolution. Skin biopsy showed a normal epidermis under which there was an interstitial infiltrate of histiocytes with degeneration of collagen as well as perivascular lymphocytic inflammation (Figure 2).

