What’s the diagnosis?
Parasites harvested from the skin

Figure 1. Irregularly shaped excoriation on the forehead.
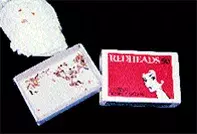
Figure 2. Material collected by the patient for expert examination.
Differential Diagnosis
Dermatitis artefacta is a condition in which skin lesions are self-induced by the patient. The lesions often have geometric outlines or telltale evidence of physical or chemical induction, but may masquerade as genuine skin disease. In contrast to the patient in this case, individuals with dermatitis artefacta deny producing the skin lesions and will often be quite vague as to how the lesions developed and will not provide elaborate details.
Neurotic excoriations are produced by patients picking, rubbing or scratching their skin. The excoriations may occur in the background of acne or a mild folliculitis, but the primary basis for the excoriations may be unclear. Fresh excoriations are often mixed with the pale scars of previous lesions. Typically the lesions are concentrated on the limbs, upper back and chest. In acne patients they may occur particularly on the face. The patient is often aware of the habit but appears compelled to continue and often seeks professional help to find a cause for the problem.
Delusions of parasitosis (monosymptomatic hypochondrial psychosis) is the correct diagnosis in this case. This condition represents a psychosis based on a false belief that no amount of rational discussion will change. Patients often complain of crawling, stinging or biting sensations and frequently collect skin debris, lint or other material in order to prove that they are infested. In some individuals this type of psychosis may develop in association with abuse of drugs, particularly cocaine. Chronic tactile hallucinosis without delusions has also been described in such people. In some patients with formication symptoms, the possibility of early multiple sclerosis may need to be excluded by careful neurological review, but these patients usually lack fixed delusional ideas. It is possible that a subset of these individuals have an ill-defined organic basis for their neurological symptoms.
Delusions of parasitosis is a difficult disorder to treat as it is necessary to establish patient trust. A thorough skin examination for scabies and careful examination of the material collected by the patient is essential. Once patient rapport has been established, some patients respond to treatment with pimozide, commencing at a dose of 1 mg per day and increasing gradually to 4 to 6 mg per day according to the response. This treatment needs to be carefully supervised as extrapyramidal or cardiac side effects may occur. Atypical antipsychotics, such as risperidone and olanzapine, have more recently been used as alternatives to pimozide and usually are used at a lower dose than with schizophrenia.
A 53-year-old woman presented with an eight-month history of a crawling sensation over her forehead. This, she explained, was caused by small parasites that were burrowing and breeding in her skin. She had managed to capture some of the parasites by digging them out of an area on her forehead (Figure 1). She had brought these parasites, wrapped in tissue paper in a matchbox (Figure 2), along with her for positive identification.

