What’s the diagnosis?
Progressive pigmented purpura

Figure 1. Irregular pigmented patches with purpura on the pretibial areas.
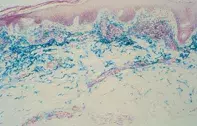
Figure 2. Skin biopsy demonstrating abundant iron deposits (coloured blue) and dermal perivascular lymphocytic inflammation with haemorrhage.
Differential Diagnosis
Necrotising vasculitis may resolve leaving extensive haemosiderin pigmentation on the shins, but the purpuric element is palpable and the pathology shows vascular necrosis and leukocytoclasis.
Traumatic haemorrhage is quite common on the anterior shins and is seen particularly in aged atrophic skin. The primary lesion is an ecchymosis, and the haemorrhage is not associated with significant inflammation.
Simple purpura usually is not limited to the lower limbs and has a short, acute history. Abnormal platelet function or thrombocytopenia may be associated, and skin biopsy reveals focal dermal haemorrhage but no significant inflammation.
Necrobiosis lipoidica is usually located on the pretibial surfaces and may appear as yellow–brown pigmented plaques with telangiectasia. The plaques are scarred and infiltrated, while skin biopsy shows a granulomatous pathology.
Pigmented purpuric dermatosis (capillaritis) is the correct diagnosis and is often a recurrent and persistent process characterised by lymphocytic inflammation of the superficial vessels and red cell leakage. A localised variant (lichen aureus) has been linked to perforating vein incompetence. Results of coagulation studies are normal but platelet function may be impaired. Hypersensitivities to khaki dyes, food preservatives, meprobamate, diuretics and nonsteroidal anti-inflammatory drugs have been implicated. Topical corticosteroid creams and pimecrolimus cream may help but the cutaneous haemosiderosis is often persistent.
Over a three-year period, a 42-year-old woman developed an asymptomatic progressive mottled yellow–brown pigmentation over her shins associated with purpura (Figure 1). The purpura fluctuated, was nonpalpable and was confined to the lower limbs. Skin biopsies showed extensive haemosiderin pigment and a superficial perivascular lymphocytic inflammatory reaction without vascular necrosis or leukocytoclasis (Figure 2).

